- Article Summary
-
Overview
As the climate crisis intensifies, its effects are not only measured in environmental degradation but also in human health and the spiraling costs associated with it. Global healthcare systems, particularly in the United States and Europe, are witnessing an upsurge in expenditures driven by climate-linked health risks. From heatwaves exacerbating cardiovascular conditions to the resurgence of infectious diseases in new regions, climate change is quietly but powerfully reshaping healthcare spending. This article dissects the mechanisms through which climate change inflates healthcare budgets, identifies the most affected populations, and explores policy responses aimed at both mitigation and adaptation.
Climate-Driven Health Conditions and Direct Costs
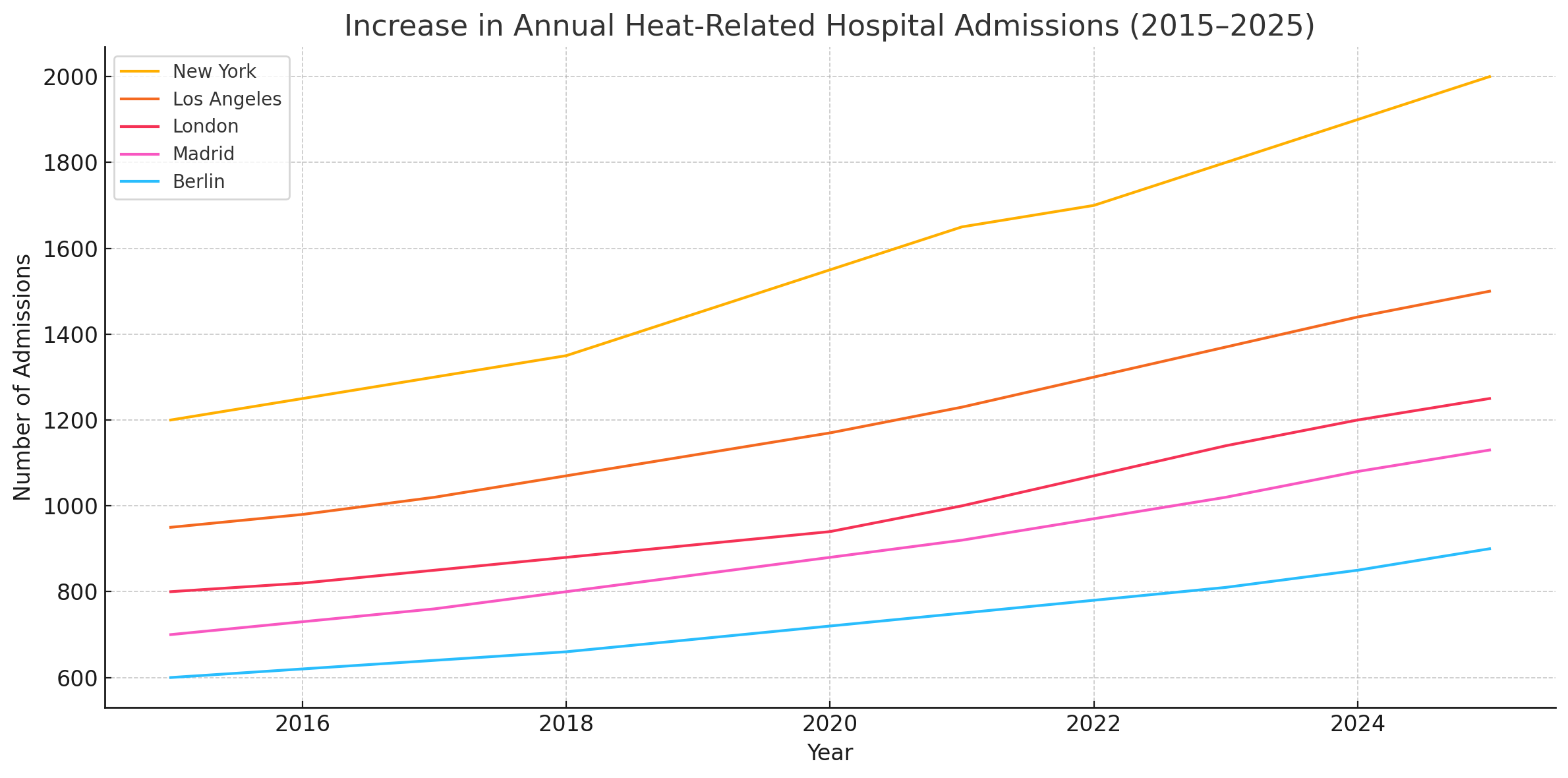
Rising temperatures have a direct impact on human health, particularly through the increase in heat-related illnesses. According to a 2025 report from the European Environment Agency (EEA), hospital admissions for heatstroke, dehydration, and exacerbated chronic conditions have grown by 14% across EU member states during the past decade. In the United States, the CDC attributes over 1,300 deaths annually to extreme heat, a number projected to more than double by 2040.
In addition to heat-related conditions, global warming is facilitating the spread of vector-borne diseases such as Lyme disease, dengue fever, and West Nile virus into regions previously unaffected. This has led to increased surveillance costs, more frequent medical interventions, and the expansion of vaccination programs, all contributing to rising healthcare expenditures. For example, the UK’s NHS has allocated an additional £200 million for climate-related disease preparedness over the next three years.
Indirect Economic Burdens on Healthcare Systems
Beyond direct treatment costs, climate change imposes significant indirect burdens. Air pollution, exacerbated by rising temperatures, is linked to respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD). According to a 2025 OECD study, air pollution-related health issues account for 7% of total healthcare costs in urban areas across developed countries.
Additionally, extreme weather events like floods, wildfires, and hurricanes disrupt healthcare infrastructure, displace populations, and strain emergency response systems. These events lead to higher insurance premiums, increased infrastructure maintenance costs, and emergency relief funding, much of which must be absorbed by public healthcare systems.
Socioeconomic and Geographic Disparities
The healthcare cost burden of climate change is unevenly distributed. Vulnerable populations including the elderly, low-income communities, and those with pre-existing health conditions face the highest risks and often have limited access to healthcare services. In southern Europe and parts of the American South, higher exposure to heat and limited medical infrastructure exacerbate health inequalities.
Moreover, individuals displaced due to uninhabitable conditions, or climate migrants, are increasing in number. These populations often require urgent medical care, vaccinations, and long-term support, placing additional stress on host countries’ healthcare systems.

Policy Responses and Investment Opportunities
Governments and institutions are beginning to act. The European Union’s “EU4Health” initiative, launched in 2025, includes a €5.1 billion allocation to strengthen healthcare systems against climate-related risks. Similarly, the U.S. Inflation Reduction Act of 2022 has spurred climate-health resilience investments, with updates in 2025 expanding funding for hospitals to upgrade cooling systems and emergency preparedness.
Healthcare providers are also exploring adaptive technologies, such as climate-resilient facility designs, AI-driven early warning systems for disease outbreaks, and telemedicine to reach vulnerable populations during climate events.
Private investors and insurers are increasingly integrating climate risk into health sector portfolios, acknowledging the economic imperative of climate adaptation. According to McKinsey’s 2025 Health Sustainability Outlook, global investments in climate-health resilience could reach $1.2 trillion by 2030.
Conclusion
Climate change is no longer a distant threat to public health; it is a present and growing financial burden on healthcare systems worldwide. With rising direct and indirect costs, and clear socioeconomic disparities, the urgency for coordinated policy, infrastructure investment, and innovation has never been greater. As we move through the 2020s, healthcare budgets must reflect not only the cost of treating illness but also the imperative of preventing climate-related health crises. In doing so, the hidden price tag of global warming may finally be brought into the light.
Why Work with ASUENE Inc.?
Asuene is a key player in carbon accounting, offering a comprehensive platform that measures, reduces, and reports emissions, including Scope 1-3, with expertise in decarbonization. Asuene serves over 10,000 clients worldwide, providing an all-in-one solution that integrates GHG accounting, ESG supply chain management, a Carbon Credit exchange platform, and third-party verification.
ASUENE supports companies in achieving net-zero goals through advanced technology, consulting services, and an extensive network.